Align staffing, compliance, and resident experience with right-sized technology, disciplined governance, and outcomes executives can defend.
January 2026 favors operators who pair empathy with rigor. In assisted living, technology is not decorating; it is a system of record, alerts, and workflows that protect residents, support staff, and satisfy regulators. The winning stack is practical—clear roles, simple integrations, and proofs you can show in a quarterly review.
Map the Stack to Operational Goals
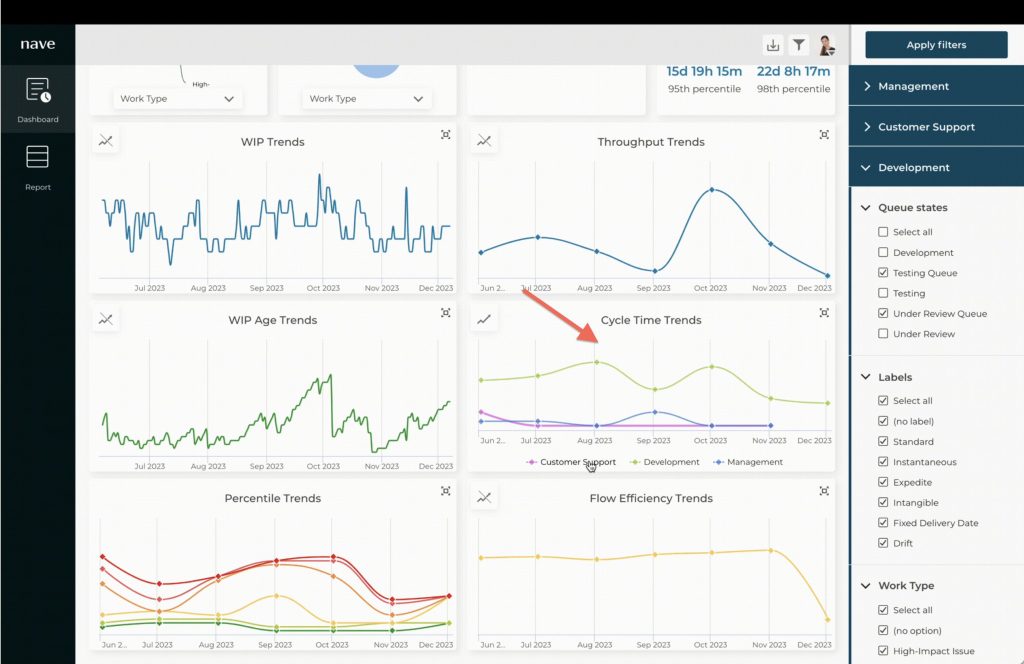
Define three goals first: staffing reliability, compliance readiness, and resident satisfaction. Select tools only when they advance these goals—scheduling and acuity tools for coverage of clarity, incident and care documentation for auditability, and communication platforms for families and physicians. Keep interfaces straightforward so frontline teams adopt without friction.
Governance: Roles, Routines, and Risk Controls
Create named ownership for each system—data steward, training lead, and compliance reviewer. Publish two routines: a weekly exception check and a monthly access audit. Add risk controls that are simple to execute: role-based permissions, consent prompts for sensitive information, and standardized note templates that create consistent records.
Interoperability and Data Hygiene
Avoid vendor sprawls. Connect critical systems through light integrations or disciplined exports and imports. Establish a data hygiene rule: no free-form identifiers, consistent resident IDs, and a quarterly archive process. A clean backbone allows faster reporting and fewer surprises during inspections.
Mini-Case: 90 Days, One Operating Sheet
A Maryland-assisted living operator planned a 90-day pilot to strengthen shift coverage and documentation. They set a single operating sheet with owners and dates, aligned the scheduling tool to acuity levels, and standardized incident notes. By the end of the quarter, callouts were better managed, and families received clearer updates. The lesson: structure and modest integrations improve outcomes without overwhelming staff.
Decision Framework: Adopt, Phase, or Park
Score each technology request across three gates—Operational Impact, Risk Reduction, and Usability. Adopt when all gates are strong, and training is feasible. Phase when the benefit is clear but change capacity is limited; deploy to one unit with weekly reviews. Parking when goals are weak or redundant is high. Document decisions with names and dates to protect schedule and accountability.

Actionable Takeaways
• Write a one-page operational brief: goals, systems, owners, and training commitments.
• Lock a biweekly governance rhythm: exceptional review and access audit with notes.
• Standardize artifacts: shift plan, incident note, family update, and monthly compliance summary.
• Establish a simple ID policy and archive process to keep resident data consistent.
• Pilot integrations where impact is highest; measure against coverage, documentation quality, and satisfaction signals.
• Run a 30-minute post-incident review to improve templates and permissions.
• Publish a quarterly technology report to leadership and families—what improved, what is next.
Technology should lighten the load, not add it. With disciplined ownership, clean data, and measured rollouts, assisted living leaders can protect residents, support staff, and demonstrate results that matter—steady coverage, clearer records, and confident audits.
Contributing Writer: Carlos Mendoza
The Guardian of Operations
Maryland
carlos.mendoza@mindyourbizexpert.com | mindyourbizexpert.com